A patent application from the Netherlands’ Leiden University Medical Center (LUMC) describes a medical apparatus that enables the resuscitation of a newborn without distancing it from its mother, while also facilitating delayed cord clamping.
Clamping and cutting the umbilical cord immediately after a baby is delivered is known to deprive them of blood rich in nutrients and oxygen. Hampering a newborn’s cardiovascular transition this way leads to a greater risk of intracranial hemorrhages, necrotizing enterocolitis, and hypotension, among others. The World Health Organization recommends clamping a child’s umbilical at least 1-3 minutes after they leave the womb.
But resuscitating a person not breathing immediately at birth must be prioritized over delayed cord clamping, per WHO guidelines. This means dealing with neonatal breathing problems can come at the cost of stable hemodynamic function for a newborn. This tradeoff likely happens too often—about 10 million of the 136 million babies born each year require respiratory assistance. This issue is just one among the many possible complications of preterm birth, or when a child is delivered before 37 weeks of pregnancy have been completed. Such occurrence is itself unfortunately quite common, affecting an estimated 15 million or more than 1 in 10 infants annually.
LUMC’s patent application is aimed at helping professionals give rapid resuscitation to newborns, particularly to preterm babies, while keeping the umbilical cord intact. Its main component is an infant-sized support platform that can be positioned as close as possible to the birth canal or abdominal opening, in case of a cesarean section birth.
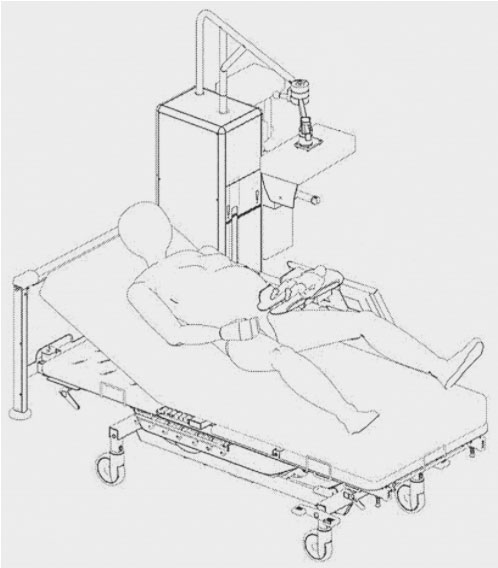
An embodiment of a resuscitation device according to the invention, in use next to a bed.
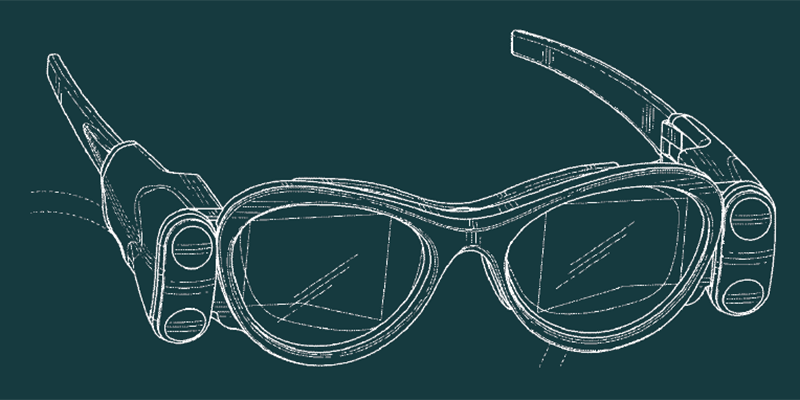
An elongated slit extends across the platform, between where the baby’s legs would go. The umbilical cord may be threaded through this space while respiratory assistance is delivered. This way, the cord may follow the shortest possible path between the placenta and the newborn.
The overall assembly would also come with a resuscitation device fully equipped to provide standard care, which includes monitoring, ventilation, heating, humidifying, and suctioning.
A monitor could display relevant resuscitation data within the line of sight of the attending neonatal caregiver, who must be NRP-certified. Information may include respiratory function, mask technique feedback, oxygen saturation, heart rate, oxygen given, and video.
Resuscitating a newborn involves a form of respiratory therapy called positive-pressure ventilation (PPV), which delivers room air or 100% oxygen to the lungs. Gases may be provided via a special mask or an endotracheal tube that bypasses parts of the anatomical airway. A neonatal caregiver may be trained to perform chest compressions on a baby or administer epinephrine, also known as adrenaline.
Temperature is also a critical factor during and after resuscitation. LUMC says its device can carry warming means: a light fixture and heating lamp above the support platform, for example. An installed humidifier may also assist in establishing thermal equilibrium. Sufficient heat is crucial to boosting an infant’s metabolic rate and oxygen consumption. Neonatal hypothermia can cause a host of vascular and metabolic complications, even death.
LUMC’s patent application features technology that could help maintain the physiological benefits of delayed cord clamping for preterm infants that are in most need. The system also serves to limit the separation between mother and child; resuscitated babies may be able to receive the immense social and physical benefits of skin-to-skin contact with minimal delay, further improving their chances in a brand new world.
The featured patent application, “Newborn Support Device and Resuscitation Device”, was filed with the USPTO on December 30, 2016 and published thereafter on July 22, 2021. The listed applicant is Academisch Ziekenhuis Leiden H.O.D.N. LUMC. The listed inventors are Arjan Benedictus Te Pas, Erwin Knoester, Franciscus Josephus Christiaan Marie Klumper, and Alexius Stefanus Nicolaas Vernooij.